State Officials Announce Latest COVID-19 Facts
Date: December 13, 2020
Number: NR20-334
Contact: CDPHpress@cdph.ca.gov
SACRAMENTO – The California Department of Public Health (CDPH) today announced the most recent statistics on COVID-19, including data on intensive care unit (ICU) capacity across the state. Based on ICU data, three regions, San Joaquin Valley, Southern California, and Greater Sacramento remain under the Regional Stay at Home Order.
Regions must remain under the order for at least three weeks and will be eligible to exit the order and return to the Blueprint for a Safer Economy only if ICU capacity projections for the following month are above or equal to 15%. The dates the following regions will be eligible to exit follow:
- San Joaquin: December 28
- Southern California: December 28
- Greater Sacramento: January 1
Under the terms of the order, when ICU capacity drops below 15% in a region, certain sectors must close by 11:59 p.m. the next day. In addition, several sectors in these regions, including restaurants, retail and shopping centers and hotels and lodging, will have additional modifications in addition to 100% masking and physical distancing requirements. Critical infrastructure, schools and non-urgent medical and dental care can remain open with appropriate infectious disease preventative measures. Details on sector closings or modifications can be found in the frequently asked questions.
Read the full Regional Stay Home Order and Supplement to the Order.
The state continues to support hospital systems and congregate care facilities across the state during as ICU capacity continues to drop. The state is providing staff assistance, personal protective gear, durable medical equipment and supplies, and infection prevention technical assistance. Yesterday, CDPH implemented a temporary waiver of nurse-to-patient ratios for intensive care units, step down units, emergency medical services and medical and surgical units. In addition, more than 300 additional medical staff has been deployed across the state, with more expected before the end of the month.
Current available ICU capacity by region:
- Bay Area: 16.7%
- Greater Sacramento Region: 15.1%
- Northern California: 29.0%
- San Joaquin Valley: 1.5%
- Southern California: 4.2%
See region map.
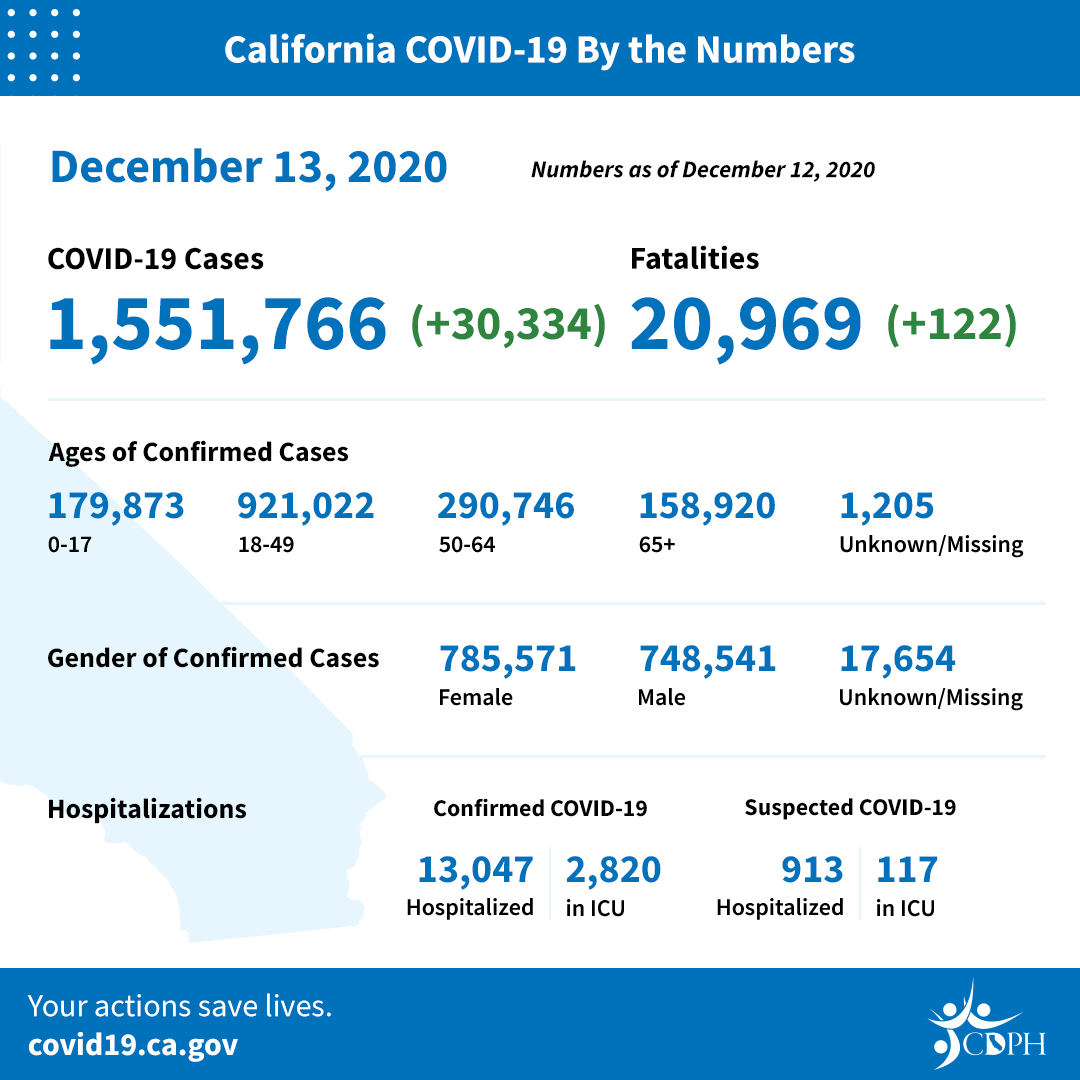
Statewide COVID-19 Data as of December 12:
California has 1,551,766 confirmed cases to date. Numbers may not represent true day-over-day change as reporting of test results can be delayed.
There were 30,334 newly recorded confirmed cases Saturday. Numbers do not represent true day-over-day change as these results include cases from prior to yesterday.
The 7-day positivity rate is 10.5% and the 14-day positivity rate is 10.4%.
There have been 27,195,587 tests conducted in California. This represents an increase of 309,457 over the prior 24-hour reporting period.
As case numbers continue to rise in California, the total number of individuals who will have serious outcomes will also increase. There have been 20,969 COVID-19 deaths since the start of the pandemic.
Testing Turnaround Time
The testing turnaround dashboard reports how long California patients are waiting for COVID-19 test results. During the week of November 29 to December 5, the average time patients waited for test results was 1.4 days. During this same time period, 58 percent of patients received test results in 1 day and 87 percent received them within 2 days. The testing turnaround time dashboard is updated weekly. At this time, all four tiers in the Testing Prioritization Guidance have equal priority for testing.
Blueprint for a Safer Economy
The Blueprint for a Safer Economy is a statewide plan for reducing COVID-19 and keeping Californians healthy and safe. The plan imposes risk-based criteria on tightening and loosening COVID-19 allowable activities and expands the length of time between changes to assess how any movement affects the trajectory of the disease. Californians can go to covid19.ca.gov to find out where their county falls and what activities are allowable in each county.
Data and Tools
A wide range of data and analysis guides California’s response to COVID-19. The state is making the data and its analytical tools available to researchers, scientists and the public at covid19.ca.gov.
Popular links include:
Multisystem Inflammatory Syndrome in Children (MIS-C)
Each week, the California Department of Public Health updates the number of cases of Multisystem Inflammatory Syndrome in Children (MIS-C) reported in the state. As of December 7, 145 cases of MIS-C have been reported statewide. To protect patient confidentiality in counties with fewer than 11 cases, we are not providing total counts at this time
MIS-C is a rare inflammatory condition associated with COVID-19 that can damage multiple organ systems. MIS-C can require hospitalization and be life threatening. Parents should be aware of the signs and symptoms of MIS-C including fever that does not go away, abdominal pain, vomiting, diarrhea, neck pain, rash, bloodshot eyes or feeling tired. Contact your child's doctor immediately if your child has these symptoms. Early diagnosis and treatment of patients is critical to preventing long-term complications.
Racial Demographics – A More Complete Picture
The California Department of Public Health is committed to health equity and collecting more detailed racial and ethnic data that will provide additional understanding for determining future action. Health outcomes are affected by forces including structural racism, poverty and the disproportionate prevalence of underlying conditions such as asthma and heart disease among Latinos and African American Californians. Only by looking at the full picture can we understand how to ensure the best outcomes for all Californians.
The differences in health outcomes related to COVID-19 are most stark in COVID-19 deaths. We have nearly complete data on race and ethnicity for COVID-19 deaths, and we are seeing the following trends: Latinos, African Americans, Native Hawaiians and Pacific Islanders are dying at disproportionately higher levels. More males are dying from COVID-19 than females, in line with national trends. More information is available at COVID-19 Race and Ethnicity Data.
Health Care Worker Infection Rates
As of December 12, local health departments have reported 59,408 confirmed positive cases in health care workers and 228 deaths statewide.
Your Actions Save Lives
California is experiencing the fastest increase in cases we have seen yet – faster than what we experienced at the outset of the pandemic and this summer. If COVID-19 continues to spread at this rate, it could quickly overwhelm our health care system and lead to catastrophic outcomes. Protect yourself, family, friends and community by following these prevention measures:
- Staying home except for essential needs/activities and following local and state public health guidelines when visiting businesses that are open.
- Following the Limited Stay at Home Order that requires all non-essential work and activities to stop between 10 p.m. and 5 a.m. in counties in the purple tier. The order took effect at 10 p.m. Saturday, November 21, and will remain in effect until 5 a.m. December 21.
- Staying close to home, avoiding non-essential travel, and practicing self-quarantine for 14 days after arrival if you leave the state.
- Keeping gatherings small, short and outdoors and limiting them to those who live in your household.
- Wearing a cloth face mask when out in public.
- Washing hands with soap and water for a minimum of 20 seconds.
- Avoiding touching eyes, nose or mouth with unwashed hands.
- Covering a cough or sneeze with your sleeve, or disposable tissue. Wash your hands afterward.
- Avoiding close contact with people who are sick.
- Staying away from work, school or other people if you become sick with respiratory symptoms like fever and cough.
- Answer the call if a contact tracer from the CA COVID Team or your local health department tries to connect. Contact tracers will connect you to free, confidential testing and other resources, if needed.
- Following guidance from public health officials.