Tuberculosis in California: 2024 Snapshot
Tuberculosis disease (TB) is an illness caused by the bacteria Mycobacterium tuberculosis. TB usually affects the lungs and spreads through the air when a person sick with TB coughs. Not everyone infected with the bacteria becomes sick. People that have been infected but are not sick have latent tuberculosis infection (LTBI). People with LTBI can become sick with TB disease in the future if they do not take treatment for LTBI.
2,109 people had TB disease in California in 2024
In 2024, 2,109 people were reported to have TB compared with 2,114 in 2023.
California's annual TB incidence was 5.4 cases per 100,000 persons; nearly double the national incidence rate (3.0 per 100,000 in 2023).
Except during the COVID-19 pandemic (2020-2022), the number of TB cases has remained consistently 2,000-2,200 cases since 2012 despite steady declines in the preceding 20 years when cases fell nearly 60% from 5,382 cases in 1992.
TB cases were reported in 45 (74%) of California's 61 local health jurisdictions (LHJs); 19 (31%) LHJs reported 1–9 cases.
The vast majority of TB cases (83%) were attributable to progression of LTBI to active TB meaning they could have been prevented with testing and treatment of LTBI. An estimated 8% of cases were in persons who arrived in California with active TB disease, and another 9% resulted from recent transmission.
The costs and consequences of TB in California are substantial. Medical and societal costs of TB reached $288 million in California in 2024.
(Costs calculated using data from Oh et al. BMC Res Notes 2017 and methods adapted from Castro et al. Int J Tuberc Lung Dis. 2016.)
TB kills more than 200 Californians each year
The percentage of people with TB who die has been significantly increasing. In 2010, 8.4% of people with TB died. In 2022, 258 (14%) people with TB died; the highest since 1995. Of those who died, 56 (22%) died before receiving treatment for TB.
People born outside the United States bear the largest burden of TB
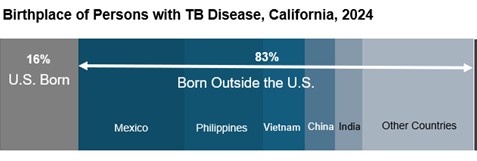
The TB rate among people born outside the U.S. (16.3 per 100,000) was 14 times higher than the rate among U.S.-born persons (1.2 per 100,000).
70% of TB in people born outside the U.S. occurred more than 5 years after U.S. arrival; nearly half occurred more than 20 years after arrival.
Among the 5 most frequent countries of birth outside of the U.S., the TB rate was highest among people born in the Philippines (41.8 per 100,000) and Vietnam (34.3 per 100,000), followed by India (21.0 per 100,000), China (16.5 per 100,000) and Mexico (12.2 per 100,000).
Severe disparities by race, ethnicity, and place of birth
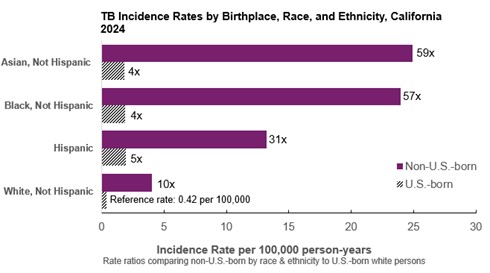
Nearly half (47%) of California’s TB cases occurred in non-Hispanic Asian persons, and 43% of cases occurred in Hispanic persons.
Rates of TB among people born outside the U.S. who are non-Hispanic Asian, non-Hispanic Black, or Hispanic were many times higher than non-Hispanic White people born in the U.S.
In each racial and ethnic group, TB rates were higher in non-U.S.-born than U.S.-born people. Among U.S.-born people, non-Hispanic Asian, non-Hispanic Black, and Hispanic persons had higher rates than non-Hispanic White persons.
Diabetes and other conditions that increase TB risk are common
41% of people with TB had diabetes, end stage renal disease, HIV infection, or another condition that can increase the risk of progression from latent to active TB disease or complicate treatment for TB and LTBI.
The most common comorbidity was diabetes mellitus, occurring in 31% of cases.
28% of persons with TB reported being current or former smokers.
HIV infection increases the risk for active TB disease, as well as for death with TB.
In 2024, 88% of patients with TB were tested for HIV. Of those tested, 74 (4.0%) were HIV-positive. The proportion of cases with HIV has fluctuated between 3.2% and 4.4% since 2015.
Among 49 people with HIV who also had a known CD4 count, 71% had a CD4 count less than 200, indicating advanced HIV infection.
TB affects children
TB in children is an indication of recent transmission particularly when it involves children under 5 years old. These young children are also vulnerable to the most severe forms of TB such as disseminated TB and TB of the central nervous system (CNS).
In 2024, there were 25 cases of TB among children under 5 years old. Of those, 2 (8%) had CNS TB.
Multidrug-resistant TB continues
Multidrug-resistant (MDR) TB is TB resistant to the two most potent first line drugs, isoniazid and rifampin. According to CDC, extensively drug-resistant (XDR) TB is MDR TB additionally resistant to fluoroquinolones and injectables, bedaquiline, or linezolid, the most potent second-line drugs.
In 2024, there were 22 (1.0%) MDR TB cases in California, a decrease from 28 cases (1.3%) during 2023. During 2020-2024, four XDR cases were reported.
The proportion of TB cases in California that are MDR has remained constant (1–2%) since drug susceptibility data began being systematically collected in 1993.
TB Outbreaks
TB can be prevented with LTBI treatment
More than 2 million Californians are estimated to have LTBI. Based on data from 2011-2012, only 23% are aware of their LTBI and only 13% have been treated.
The majority of people with LTBI (1.8 million) likely acquired their infection while living outside the U.S.
An estimated 83% of TB cases occur because of progression from LTBI. This means that testing for and treating LTBI will prevent many TB cases in California.
AB 2132, a new law that took effect in 2025, requires adult patients receiving primary care services to be offered a TB test if TB risks are identified, followed by provision or referral for appropriate follow-up care.
CDPH has created a set of TB resources and tools for providers.
CDPH has released a comprehensive report on LTBI in California (PDF, 4.8 MB).
The U.S. Preventive Services Task Force recommends testing and treating for LTBI for persons at increased risk of LTBI.
Risk assessment tools are available for use by medical providers to identify persons at risk for LTBI for testing and treatment.
National guidelines recommend shorter treatment for LTBI (CDC LTBI Guidelines webpage), (NTCA/NSTC LTBI Clinical Recommendations).
This document reflects data as of July 27, 2025.