Thank you to the healthcare providers in California for your tireless work in helping to keep California safe and providing healthcare access to all who need it. This alert provides additional guidance for California healthcare providers in the evaluation and management of suspected monkeypox cases.
I. Situation Summary as of May 27, 2022
The California Department of Public Health (CDPH) continues to work with local health departments (LHDs) and California healthcare providers on the ongoing domestic monkeypox situation. As of May 27, one confirmed case of monkeypox has been identified in California. Local health departments (LHDs) are working with health care providers to evaluate persons with possible monkeypox. Health care providers should notify their Local Health Department (LHD) immediately of any possible cases of monkeypox.
II. Recommendations for the evaluation of a possible monkeypox case
CDPH requests that health care providers report cases of persons meeting the definition of a Possible Case (Appendix) immediately to their LHD: LHD Contact Information (ca.gov).
The classic presentation of monkeypox disease includes a flu-like illness lasting a few days, followed by a characteristic rash. Presenting symptoms typically include fever, chills, a distinctive rash, and/or new lymphadenopathy; however, onset of perianal or genital lesions in the absence of flu-like symptoms has been reported. The rash may affect the face and extremities (including palms and soles). Mucous membranes and genitalia may be involved. The appearance and progression of the rash is very characteristic, evolving sequentially from macules (lesions with a flat base) to papules (slightly raised firm lesions), vesicles (lesions filled with clear fluid), pustules (lesions filled with yellowish fluid), and crusts which dry up and fall off.
When evaluating a patient that you suspect may have monkeypox infection, please consider the following.
1. Suggestive history includes:
- recent travel to Central or West African countries or other areas reporting monkeypox cases; and/or
- contact with a person or people who have a similar appearing rash or who received a diagnosis of confirmed or probable monkeypox and/or
- is a man who regularly has intimate in-person contact with other men,
2. Physical exam:
- The rash associated with monkeypox involves vesicles or pustules that are deep-seated, firm or hard, and well-circumscribed; the lesions may umbilicate or become confluent and progress over time to scabs. (Figure 1)
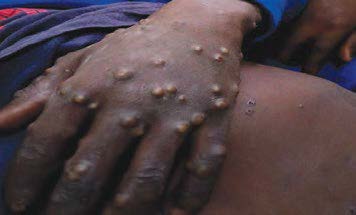
Figure 1: Vesiculopapular rash of monkeypox. Source; Nigerian Centre for Disease Control
- The rash associated with monkeypox can be confused with other diseases that are encountered in clinical practice, especially in the genital or perianal areas (e.g., secondary syphilis, herpes, chancroid, molluscum contagiosum, and varicella zoster). However, a high index of suspicion for monkeypox is warranted when evaluating people with a characteristic rash, particularly for men who report intimate contact with other men and who present with lesions in the genital/perianal area, travel to an areas where monkeypox cases have been reported in the month before illness onset, or contact with a person either with a similar rash or who is a suspected or confirmed case of monkeypox.
III. Recommendations for Monkeypox Virus Testing
Initial testing for monkeypox virus is done in specialized laboratories that are capable of conducting orthopoxvirus PCR. Confirmatory testing is done at CDC using a specific monkeypox virus test. It is important to work with your LHD in order to ensure the proper collection, handling, and submission of specimens.
If a patient is evaluated and monkeypox is considered to be high on the differential diagnosis consult with your LHD on testing. If lesions are present on different parts of the body, collect specimens from different locations on the body and/or from lesions with different appearances. If f only 1 location is affected, collect specimens from more than 1 lesion. Collect specimens as follows: 1) Vigorously swab or brush lesion (unroofing, if possible) with two separate sterile dry polyester or Dacron swabs; 2) Break off end of applicator of each swab into a separate sterile 1.5- or 2-mL screw-capped tube with O-ring or place each entire swab in a separate sterile container. Note that 2 specimens should be collected from each lesion sampled. Keep swab dry and do not add or store in viral or universal transport media. Contact your LHD for specific instrutions on how to submit the specimens to the testing laboratory. Please see additional details at:
Preparation and Collection of Specimens | Monkeypox | Poxvirus | CDC
Laboratories in California will perform a test for orthopox virus to assess for monkeypox on one set of specimens, and CDC will perform confirmatory monkeypox testing on a second set of specimens if orthopox testing is positive.
In addition to collecting specimens for monkeypox virus testing, please rule out and test for other more common causes of the rash as clinically indicated, including syphilis, herpes, and varicella zoster, etc.
IV. Infection Control Considerations for Suspected Monkeypox Cases
Patients presenting with suspected monkeypox should be placed as soon as possible in a single-person exam room with door closed, or an airborne infection isolation room, if available. The patient should remain masked, as tolerated with a respirator or surgical mask (as currently required for all persons in healthcare settings) and any exposed skin lesions should be covered with a bandage, sheet, or gown. In addition, please consider telemedicine evaluation in a medically stable patient, in order to mitigate the risk of spread to healthcare personnel (HCP) and other patients.
HCP evaluating patients with suspected monkeypox should wear the following personal protective equipment (PPE): gloves, gown, eye protection (goggles or faceshield) and a N95 or equivalent or higher-level respirator. HCP should don PPE before entering the patient’s room and use during all contact with the patient. HCP should remove and discard gloves, gown and eye protection, and perform hand hygiene prior to leaving the patient’s room; the N95 respirator should be removed, discarded and replaced with a mask for source control after leaving the patient’s room and closing the door.
Any EPA-registered hospital-grade disinfectant can be used for cleaning and disinfecting environmental surfaces. Take care when handling soiled laundry (e.g., bedding, towels, personal clothing) to avoid contact with lesion material. Soiled laundry should never be shaken or handled in manner that may disperse infectious particles.
CDC has posted guidance on monkeypox exposure risk assessment and monitoring of exposed individuals, including HCP.
V. Monkeypox Treatment and Management Considerations
Most patients have mild disease and recover without medical intervention. The current circulating strain of monkeypox appears to be the West African clade, which tends to cause milder disease. Although information is limited, many identified patients appear to have been managed in the outpatient setting. Hospital admission for supportive care may be necessary in patients who develop more severe illness. Bacterial superinfections should be appropriately managed, but may be difficult to distinguish from viral inflammation.
Antiviral therapy of cases or post-exposure prophylactic immunization of contacts may be considered after consultation with the LHD, CDPH, and CDC. Supplies of the products are only available from the federal Strategic National Stockpile.
- The antiviral tecovirimat, licensed by FDA in 2018 to treat smallpox, can be considered to treat monkeypox disease that is severe. Additional guidance from CDC on its use is anticipated shortly.
- Two vaccines licensed by FDA can be considered for post-exposure prophylaxis in people who have had a high risk exposure to monkeypox, as defined by CDC.
- JYNNEOS is a live, non-replicating vaccine
- ACAM2000 is a live replicating vaccine.
Vaccine should be given within 4 days of exposure to prevent disease but might reduce severity of disease up to 14 days after exposure. Additional guidance from CDC on the use of vaccines for post-exposure prophylaxis in the outbreak is anticipated shortly.
A recent clinician-focused presentation on the current monkeypox situation has been recorded and is available on the CDC website.
VI. Key Messages and Resources for Patient Education
Communicating monkeypox-related risks, prevention, detection, and care is essential for preventing further spread of monkeypox and controlling the current outbreak, particularly for at-risk and affected communities. As of now, the communities most impacted by this outbreak are among gay, bisexual, and other men who have sex with men (MSM).
Due to the media attention on this outbreak, patients may have questions and be seeking evaluation for monkeypox if they are experiencing a rash or other symptoms. Providers should communicate relevant, non-stigmatizing and non-judgmental health information and advice when serving all patients but particularly patients who may already feel stigmatized by circulating misinformation such as MSM and African/Black populations.
Key messages include the below:
- Prevention – any person (of any gender or sexual orientation) who has direct contact with an infected person, including skin-to-skin and/or sexual contact, can get monkeypox. Steps for self-protection include asking intimate and other sexual partners about symptoms, avoiding skin-to-skin or face-to-face contact with anyone who has symptoms, keeping hands clean with water and soap or alcohol-based hand rub, and maintaining respiratory etiquette.
- Detection and care – currently, a person with monkeypox is considered infectious when they have symptoms. If a person with monkeypox or their recent sexual partners (from the last 21 days) have unusual sores or a rash, especially if accompanied by fever or a feeling of discomfort or illness, they should contact their health care provider and be evaluated for monkeypox. If someone is suspected or confirmed as having monkeypox, they should isolate, abstain from sex (including oral sex) and avoid sharing bedding, towels, and clothing until the scabs have fallen off and fresh skin has formed underneath. During this period, patients can get supportive treatment to ease monkeypox symptoms. Anyone caring for a person sick with monkeypox should use appropriate personal protective measures, including wearing a mask and gloves and cleaning objects/surfaces that have been touched.
- Reporting - Any rash-like illness consistent with the clinical descriptions above during travel or upon return should be immediately reported to a health care professional, including information about all recent travel, sexual history, and smallpox immunization history.
For additional messaging on monkeypox for gay, bi, and trans men who may be exposed through sex or intimate contact, please visit the Building Health Online Communities website. Clinicians can also use the MSM Toolkit: A Clinician’s Resource for Sexually Transmitted Diseases in Gay Men and Other Men Who Have Sex with Men as an additional resource.
VII. Background
The California Department of Public Health (CDPH) issued an advisory on May 20, 2022 to supplement the information contained in the Health Alert issued by the U.S. Centers for Disease Control and Prevention(CDC) to provide additional guidance to California LHDs and health care providers. This is the second in a series of ongoing updates.
Monkeypox is a viral zoonosis with symptoms very similar to, though clinically less severe than, those seen in the past with smallpox infections. Monkeypox virus belongs to the Orthopoxvirus genus which also includes the variola (smallpox) virus. Monkeypox occurs primarily in Central and West Africa and has been rarely exported to other regions. Nigeria, in particular, has had a large outbreak of monkeypox, with hundreds of cases to date. The wild animal reservoir is unknown.
After an average incubation period of 6 to 13 days (range, 5 to 21 days), flu-like symptoms may appear, and may include fever, headache, lymphadenopathy, myalgia, and fatigue. This is followed approximately 1 to 3 days later with rash that may affect the face and extremities (including palms and soles). Mucous membranes and genitalia may be involved. The appearance and progression of the rash is very characteristic, evolving sequentially from macules (lesions with a flat base) to papules (slightly raised firm lesions), vesicles (lesions filled with clear fluid), pustules (lesions filled with yellowish fluid), and crusts which dry up and fall off.
Cases of monkeypox outside of Western and Central Africa are extremely rare. In 2021 there were two travel associated cases identified in the US, and prior to that the most recent cases were identified in 2003 during an outbreak of 47 cases associated with imported small mammals. Cases of monkeypox have been identified in several non-endemic countries since early May 2022; many of the cases have involved men who have sex with men (MSM) without a history of travel to an endemic country.
In the most recent reported cases, flu-like symptoms may not have always occurred; some recent cases have begun with characteristic, monkeypox-like lesions in the genital and perianal region, in the absence of subjective fever and other flu-like symptoms. A person is considered infectious from the earlier date of either the onset of flu-like symptoms or the onset of the rash. Infected persons are presumed to remain infectious until lesions have crusted, those crusts have separated, and a fresh layer of healthy skin has formed underneath.
Human-to-human transmission likely occurs primarily through large respiratory droplets that typically do not travel more than a few feet, so prolonged face-to-face contact is required. Other human-to-human transmission can occur through direct contact with body fluids or lesion material, and indirect contact with lesion material, such as through contaminated clothing or linens.
Confirmatory laboratory diagnostic testing for monkeypox is performed using real-time polymerase chain reaction assay on lesion-derived specimens for orthopox virus, with confirmatory monkeypox virus testing at the CDC.
There is no specific treatment for monkeypox virus infection, but particularly in the outbreak setting, post-exposure smallpox vaccine and case treatment with antivirals may be considered after consultation with CDPH and CDC. Monkeypox is usually self-limited with disease symptoms lasting 2 to 4 weeks. Complications, including secondary infections, are possible. In Africa, recent fatality rates of 3-6% have been reported by the World Health Organization; the West African clade of monkeypox virus that has been isolated in California is generally considered milder.
VII. Additional Information and Resources
https://emergency.cdc.gov/coca/calls/2022/callinfo_052422.asp
HAN Archive - 00466 | Health Alert Network (HAN) (cdc.gov)
2022 United States Monkeypox Case | Monkeypox | Poxvirus | CDC
https://www.cdc.gov/hai/pdfs/ppe/PPE-Sequence.pdf
https://www.who.int/news-room/fact-sheets/detail/monkeypox
BHOC Monkeypox Information for Gay, Bi, and Trans People Who May Be Exposed Through Sex and Intimate Contact
Information For Clinicians | Monkeypox | Poxvirus | CDC