Background
The California Department of Public Health (CDPH) warns healthcare providers about an increased number of reported cases of coccidioidomycosis with onset dates in 2023. Healthcare providers should consider testing for coccidioidomycosis in patients who present with compatible symptoms and risk factors.
Situation
A total of 9280 cases of coccidioidomycosis with onset dates in 2023 have been reported in California to date (Figure 1). This case count is higher than the final case count in any other year since coccidioidomycosis cases became individually reportable in California in 1995.
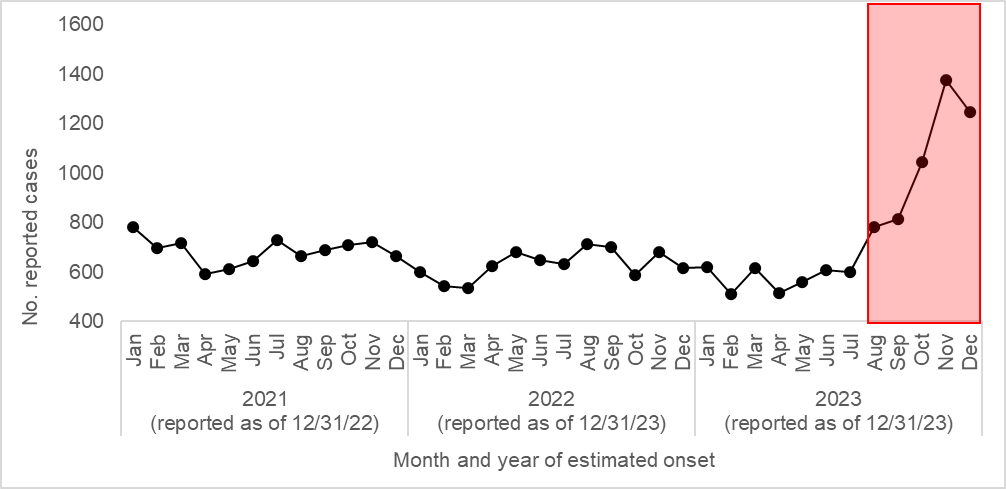
Furthermore, unlike the prior two years, most 2023 cases (5,185, 57%) were reported from August–December 2023, with sharp increases in October through December (Figure 2). As noted in an earlier CDPH press release, heavy rainfall in the winter of 2022-2023 following years of drought was predicted to lead to increases in coccidioidomycosis cases across California in 2023, particularly in the late summer and fall. We expect to continue to receive a higher number of case reports than usual throughout the winter months of 2024. While the recent rains should decrease the risk of new infections, persons who have been infected in prior weeks and months will continue to present for care.
: Reported coccidioidomycosis by year of estimated onset, California, 2001-2023 (Preliminary data for 2023 in red, reported as of December 31, 2023)
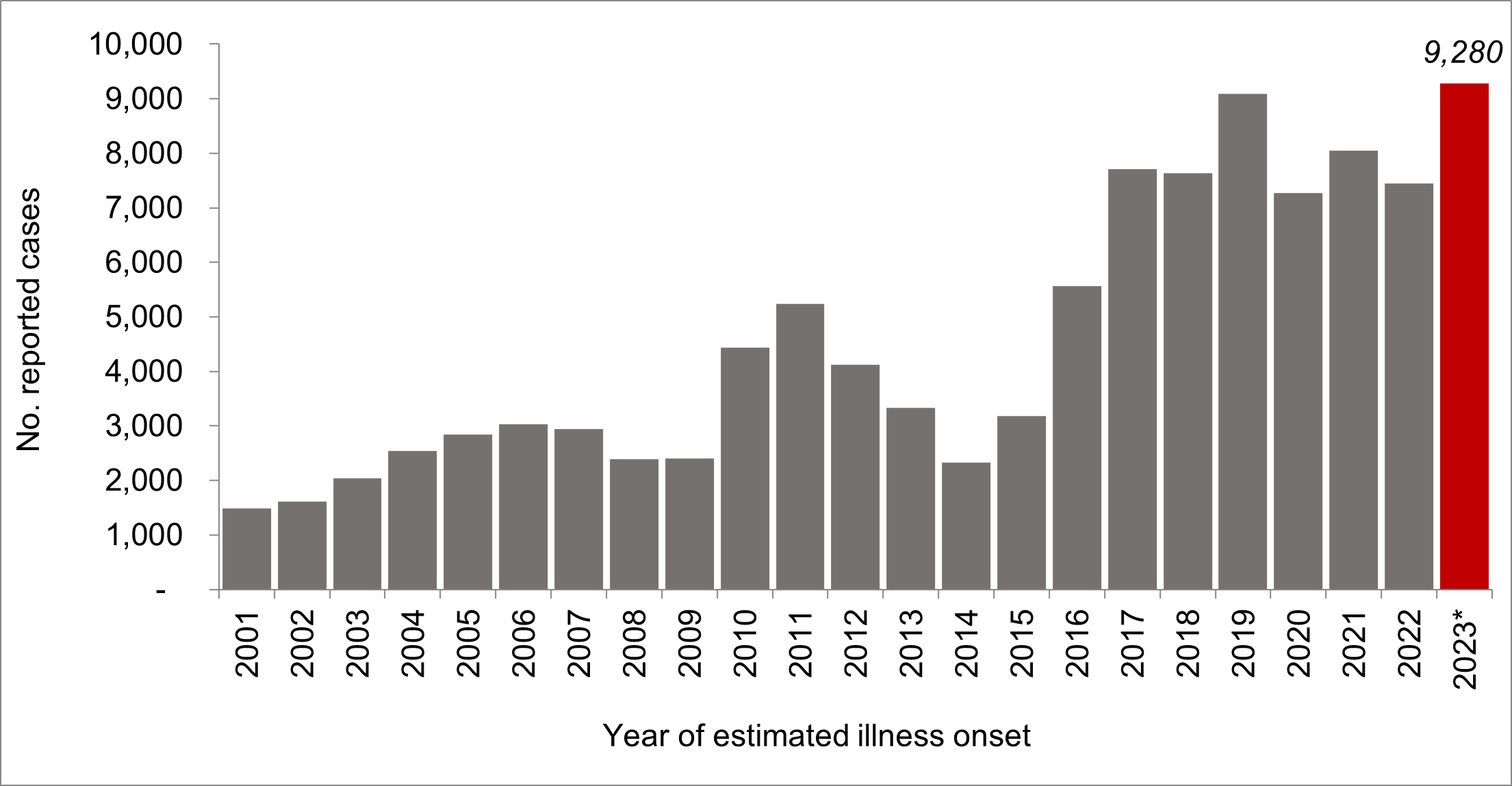
*Data from 2023 is provisional, and is likely an underestimate due to lags in data reporting and lack of complete data for December.
: Reported suspect, probable, and confirmed cases of coccidioidomycosis by month and year of estimated onset, California 2021-2023
 Coccidioidomycosis Overview
Coccidioidomycosis Overview
Coccidioidomycosis (also called Valley fever or “cocci”) is a disease caused by inhalation of the spores of the Coccidioides fungus that grows in the soil and dirt in some areas of the southwestern United States, with 97% of cases reported in Arizona and California. Anyone who lives, works, or travels in areas where Coccidioides is present can become infected, particularly people exposed to dirt and dust outdoors. Coccidioidomycosis may be asymptomatic but typically presents as a self-limited respiratory illness or pneumonia. Patients may also present with erythema nodosum. However, infection can also lead to progressive pulmonary disease or severe disseminated disease including meningitis and can be fatal.
Pulmonary coccidioidomycosis is commonly misdiagnosed because it is difficult to differentiate from other respiratory diseases through symptoms alone, and patients are often treated with antibiotics (up to 70% of patients with coccidioidomycosis receive antibiotics within the 3 months prior to diagnosis). Antibacterial agents are not effective against coccidioidomycosis, and coccidioidomycosis should be considered in patients with respiratory symptoms, especially pneumonia, who fail to improve on antibiotics.
Changes in Geographic Distribution
Climate change may be impacting the distribution and burden of Coccidioides within California, given the substantial increase in cases in recent years. Historically, coccidioidomycosis rates in California are consistently highest in the Central Valley and Central Coast regions. However, rates have recently increased most in the Northern San Joaquin Valley and in Southern California, suggesting expansion of Coccidioides into new emerging regions (Figure 3).
: Coccidioidomycosis incidence rates by county, California, 2001—2022*
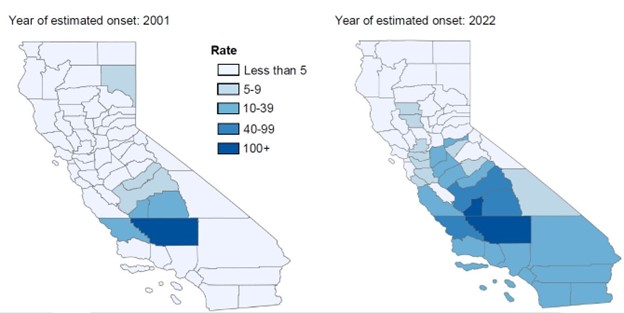
* Map for 2023 is unavailable as 2023 case counts are preliminary and subject to change
Recommendations
Recommendations for Healthcare Providers
Consider Cocci!
Winter is respiratory virus season, and many patients will be presenting with respiratory symptoms that could be attributable to a variety of pathogens. However, given the increase in coccidioidomycosis cases state-wide, clinicians should consider coccidioidomycosis as a potential diagnosis when evaluating a patient with community acquired pneumonia or respiratory illness living in or returning from endemic or emerging regions. Ask about travel history and occupation to determine potential risk factors (e.g., exposure to high incidence area, exposure to outdoor dirt/dust).
- Consider coccidioidomycosis in patients who:
- Live, work, or travel in areas with coccidioidomycosis.
- Are exposed to outdoor dust or dirt.
- Are symptomatic for a week or longer.
- Are not responding to standard treatment for CAP.
Early diagnosis for coccidioidomycosis can reduce unnecessary antibiotic use, lower the risk of progression of untreated disease, and improve the likelihood of patients receiving appropriate treatment and management.
Disseminated coccidioidomycosis and coccidioidal meningitis comprise <1% of diagnosed cases. However, with the increased number of cases in California, healthcare providers should be alert for these more severe presentations of coccidioidomycosis.
Testing and Management
Diagnosing coccidioidomycosis is challenging, but important as a delayed or missed diagnosis can delay proper management and may result in poor outcome. The diagnosis of coccidioidomycosis relies primarily on serology, which can be difficult to interpret. If you order serologic tests to detect Coccidioides IgM and IgG antibodies, please consider the following:
- Enzyme immunoassay (EIA), immunodiffusion (ID), and complement fixation (CF) tests are the most used coccidioidomycosis serologic tests and have variable sensitivities and specificities.
- A negative result from one test type does not necessarily invalidate a positive result from another test type.
- Not all patients with coccidioidomycosis will have a detectable CF titer.
- A patient with a positive Coccidioides IgM OR IgG (or both) could have acute coccidioidomycosis.
- Depending on factors such as the timing and level of exposure and patient immune status, antibody development may lag illness onset by several weeks.
- If there is high clinical suspicion of coccidioidomycosis, clinicians can consider repeating serologies 2-4 weeks later or utilizing histopathology, polymerase chain reaction (PCR) testing, or culture.
- Recent cases of severe coccidioidomycosis have been identified with positive cultures but negative serologies. For patients hospitalized with suspected severe coccidioidomycosis, PCR and culture of tissue or respiratory specimens should be considered, particularly if serologies are negative.
- PCR tests may detect Coccidioides in respiratory or cerebral spinal fluid specimens earlier in the course of illness, and with a faster turnaround time than culture, but may not be widely available.
- Culture growth may take up to a week, and processing and manipulation of cultures should be done in a biosafety level 3 laboratory.
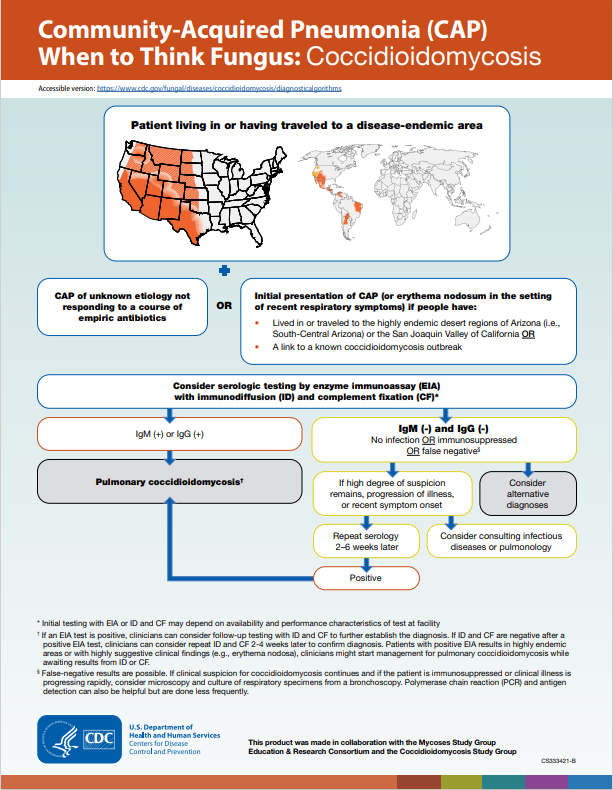
The CDC algorithm for coccidioidomycosis evaluation is included below (Figure 4).
: CDC algorithm for consideration of coccidioidomycosis as an etiology of community acquired pneumonia.
Treatment
Treatment decisions can be complex, and range from supportive care to antifungal agents, depending on the presence of symptoms, severity of disease, and medical comorbidities of the patient. Consider consultation with an infectious diseases physician or pulmonologist.
For additional guidance on testing and management, refer to the CDC website and IDSA guidelines for coccidioidomycosis.
Resources
Health care providers can reference the latest guidance on diagnosing and managing Valley fever at the resources below: