Medicare Premium Payment Program (MPPP)
Medical Out–of–Pocket (MOOP) Program
Program Benefits
Who is covered?
ADAP clients who are also receiving health insurance premium payment assistance through the MPPP program.
What is covered?
Outpatient expenses that count towards your insurance plan's out-of-pocket maximum, which are the copayment, coinsurance, and deductible for medical care as part of the policy's covered benefits.
Note: All claim submissions must be for expenses incurred during your active MPPP eligibility period.
Billing and Claim Submissions
Obtaining required supporting documentation for services received
- Provide the medical provider with the PAI-CDPH identification card.
- Request a medical billing statement or invoice from the provider.
- After the client's appointment, the client should receive an Explanation of Benefits (EOB) from their insurance company.
Note: If the client does not receive an EOB, they should contact their insurance company to request one. If the client has difficulty obtaining an EOB, please contact PAI directly at (877) 495-0990 for further instruction on acceptable submission documentation.Submitting a Claim to PAI
To submit a claim to PAI, the following must be included:
Note: One Medical Out-of-Pocket Claim Form is required for each date of service and provider. For example, if the client visits multiple providers on the same day, they will need to submit each claim individually.
Claims can be sent using one of the following methods:
Client
| Paper
| Complete and submit CDPH MOOP Claim Form, supporting documentation such as invoice or receipt, and Explanation of Benefits from insurance plan to CDPH's Medical Benefits Manager, Pool Administrators, Inc. (PAI) at:
|
Provider
| Paper
| Complete and submit CDPH MOOP Claim Form, supporting documentation such as invoice or receipt, and Explanation of Benefits from insurance plan to PAI at:
|
Provider
| Electronic
| Call PAI customer service at (877) 490-0990 to establish electronic claims submission and automated payments.
Use payer ID PAI02 when submitting electronic claim forms for MDPP clients.
|
Reimbursement
How will the client be reimbursed?
PAI pays the reimbursement directly to the provider.
If the client is required to pay at the time of service, one of the following should occur:
- Provider issues the reimbursement directly to the client, or
- Provider will apply the reimbursement as a credit on the client's account.
If the client is not required to pay at the time of service, one of the following should occur:- The provider should work directly with PAI and submit the claim on the client's behalf for payment, or
- The client submits the claim and PAI will submit the payment on the client's behalf.
Claim Denial
What could cause a claim to be denied?
- Ineligible dates of service
- Unauthorized expense: not covered by medical insurance
- Any expense that is listed as "Not Covered by the Primary Insurer". For example, elective outpatient surgeries may not be covered by primary insurance and would not be reimbursable by CDPH.
- Unauthorized expense: medical service is out of network
- Unauthorized expense: Inpatient service
- Service does not count toward your annual out of pocket maximum
- Client name does not match the invoice
- Supporting documentation not provided within 21 days of the Information Request letter being sent
- Cost of Service does not match the supporting documentation
- Other
Note: If a client receives a denial letter, they have 20 days from the date of the letter to file an appeal.Request for More Information (See image 4)
A client may receive a request for more information in the following circumstances:
- Supporting documentation was not provided
- Supporting documentation is incomplete. Please send provider billing invoice
- Supporting documentation is incomplete. Please send insurance Explanation of Benefits
- Supporting documentation is illegible
- Supporting documentation does not match date of service
- Supporting documentation does not match submitted request
- Supporting documentation does not match requested claim reimbursement amount
- Other
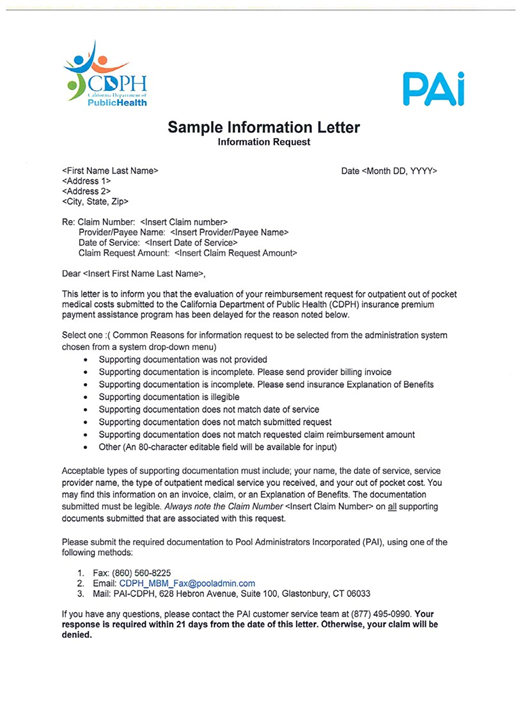
Note: A client has 21 days from the date of the letter to provide PAI with the requested documentation. Reminder: A provider is not obligated to waive any co-payments that are due at the time of service. If the client's provider does require payment at the time of service, the client is encouraged to ask the provider to contact PAI directly to discuss the program in more detail. Additionally, in accordance with IRS guidelines, providers are required to submit completed W9s to PAI prior to PAI remitting payment. PAI will contact the provider to obtain the W9 if one is not already on file.Image 1: Sample Medical Out-of-Pocket Claim Form
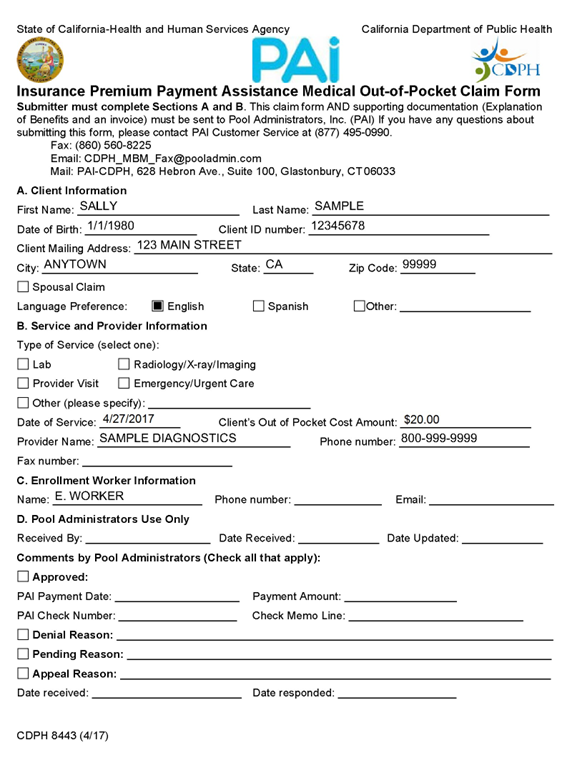
Image 2: Sample Invoice
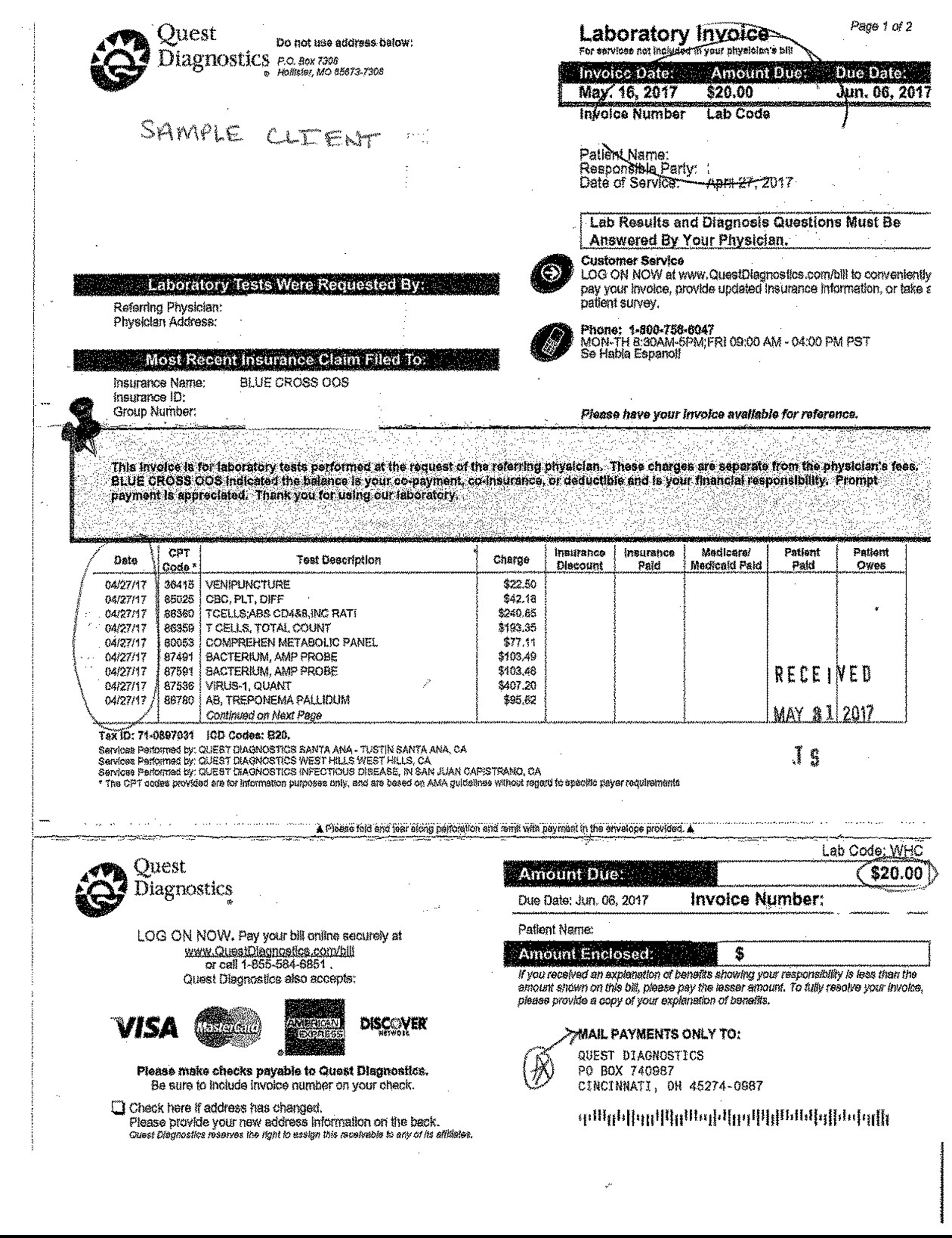
Image 3: Sample Explanation of Benefits (EOB)
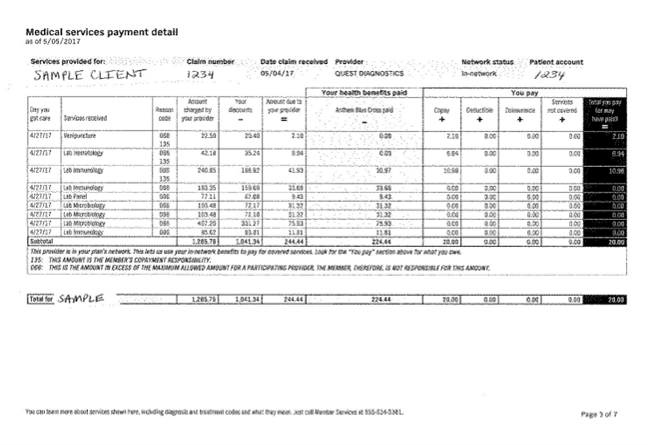
Image 4: Sample Information Request Letter